Prostate Cancer Survivorship
The history of cancer goes back to ancient times. As a species, we have struggled to understand it, to control it, to prevent and treat it — to survive it. Ancient Egyptians blamed the gods. Hippocrates, often called the founder of modern medicine, believed that cancer was caused by an imbalance of ‘black bile’ in the body. He used the Greek term for crab ‘karkinos’ (carcinos) to describe cancer, and we see this terminology still in use today. Cancer was considered incurable. In the 1800s, when anaesthesia became available, surgery as a method for treating cancer escalated, and in the early 1900s radiation therapy emerged. These two treatment methods dominated cancer therapy until around the 1960s. Chemotherapy as a cancer treatment rapidly expanded after World War II. Hormone therapy also came into the cancer war chest in the mid-1900s, and in 1966 Charles Huggins won a Nobel Prize in Physiology or Medicine for his discoveries concerning hormonal treatment of prostatic cancer. While all these important medical developments were happening however, the perspective of the patient themselves was not a clear area of focus. This started to change in the late 1980s. The idea that the quality of life of the patient and their experience of cancer mattered became a topic of discussion.
One key event was in 1986 when the National Coalition for Cancer Survivorship (NCCS) was founded by cancer survivors in the United States to advocate for all people affected by cancer. The NCCS defined survivorship as extending from the time of diagnosis and for the balance of life, a definition then expanded to include family, friends and caregivers. It took another ten years before major health bodies, such as the National Institutes for Health National Cancer Institute, noticeably took on the idea of cancer survivorship. And while now many national and international health organisations talk about improving quality of life and the patient and family experience of cancer, they are about 70 years behind what people with cancer have been asking for and doing themselves to achieve this goal.
In a relatively recent example, the incidence of prostate cancer in Australia dramatically increased in the early 1990s as a result of the introduction of the prostate-specific antigen blood test as the first (and still only, although now more refined) way to detect prostate cancer early, when it is potentially curable. At this time, information and support services for men with prostate cancer were very hard to find, and so men themselves in a grassroots movement established community-based support groups all over the country, supporting each other and lobbying hard for improvements in services and treatments. Connected to this was the formation of the Prostate Cancer Foundation of Australia in 1996, and in time the two movements merged to become the one peak voice for men with prostate cancer and their families.
Treatments for prostate cancer have dramatically changed over the past two decades. Robot-assisted surgeries, refined methods of radiation therapy, a range of different hormone-blocking treatments, new chemotherapy regimens, and targeted or personalised medicine that may be prescribed based on genomic profiling are now available in many, although not all, settings. Despite all these positive developments, research shows that men and their doctors, and the nurses and allied health professionals who look after them, report the experience of prostate cancer as being challenging, medically focused, and uncoordinated, with men’s support needs often still not being adequately met. In all of this medical progress, change and evolution, the patient experience should be the central focus. Patient priorities and preferences should guide each step and each decision. Survivorship matters. So what do we need to do?
In 2019 a 47‐member expert panel was convened that included leaders from key Australian and New Zealand clinical and community groups and consumers from diverse backgrounds, including LGBTQIA people and those from regional, rural and urban settings. Panel members included urologists, medical and radiation oncologists, GPs, nurses, and physiotherapists from organisations including Cancer Council Australia, Peter MacCallum Cancer Centre, Cancer Voices New South Wales, Prostate Cancer Foundation of Australia, Urological Society of Australia and New Zealand, Psychology Board of Australia, Flinders Centre for Innovation in Cancer, Australian Prostate Centre, Medical Oncology Group of Australia.
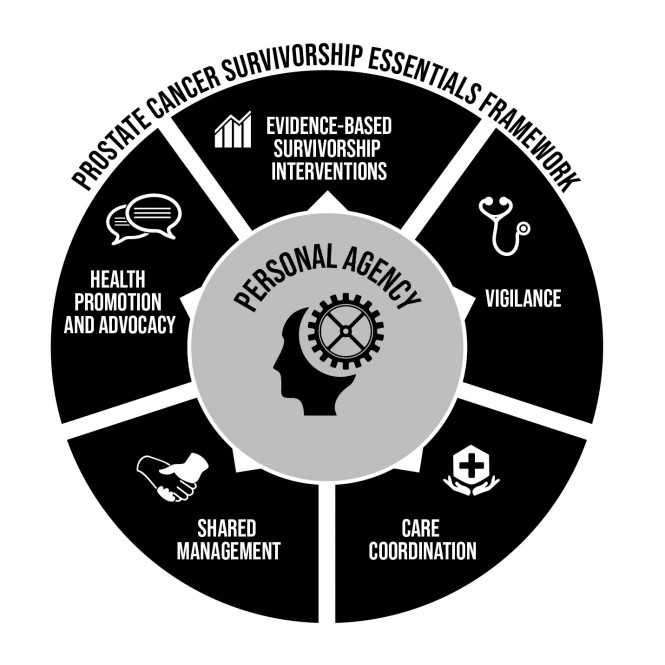
Using online surveys and a face-to-face meeting throughout 2019 and 2020, descriptors for men’s current prostate cancer survivorship experience were generated, along with survivorship elements that were assessed for importance and feasibility. From these, six key aspects of survivorship that both men with prostate cancer and their health care team agree about were identified:
• Health Promotion and Advocacy
• Shared Management
• Vigilance
• Personal Agency
• Care Coordination
• Evidence-based Survivorship Interventions.
So what does this all mean?
Health Promotion and Advocacy
For men and their partners, Health Promotion and Advocacy means having accurate information about prostate cancer for yourself, your family and your community. This also means advocating for better treatment and services when needed. And it means taking a men’s health approach to prostate cancer where all aspects of your health and wellbeing matter.
What can I do? Be informed and be active in seeking information from credible and reliable sources such as those listed in the Appendix of this book. Share what you know about prostate cancer with people who matter to you, in your family and close networks. Help raise the profile of prostate cancer, so it is a topic we can all talk about as an important men’s health issue. Encourage other men to be proactive about their health and understand about their prostate cancer risk. Perhaps connect with local support groups in your area and see how you might help. Support the Prostate Cancer Foundation of Australia in its work to improve this area of men’s health. Be informed. Add your voice to the community conversation about prostate cancer. Be heard.
Shared Management
This means being an equal partner in your health care, sharing decision-making with your health care team and sharing how you will tackle challenges as they arise. Being an equal partner starts at the beginning with informed decision-making around testing and treatment, understanding and managing the physical and psychosocial effects of treatment and of the disease at every stage of the disease.
What can I do? Be clear with your health care team about how involved you want to be in decisions about your care, and who else you want to be involved, such as your partner or other family members or supports. Question lists can help guide the conversation with your doctor, nurse or other health professional and are a great memory guide. Plan in advance of your consultation with your doctor and work out what questions you need answered, perhaps with the support of a partner or a close friend. Being informed will help you be more action-oriented in how you work with the team. Make sure your family doctor is also connected into the team so that they are well prepared to support you.
Vigilance
Vigilance refers to the clinical surveillance of patients from health professionals across the survivorship experience from diagnosis and through life, and this includes not only physical issues such as the control of the cancer and management of physical side effects but also other illnesses that can occur as we age. This also includes checking on your emotional and social wellbeing.
What can I do? Communicate your concerns and how you are going both physically and emotionally to your health care team. They might not always pick up on your concerns and they can’t read your mind. Don’t assume the effects or issues you are concerned about are not important or that your doctor or nurse is not interested or too busy to help. If it matters to you, then it matters to your health care team. How do you think you are going? There are tools around to help gauge your level of stress. For example, there is a ‘Distress Thermometer’ that has a symptom checklist with it, and a link to this is in the Appendix. Your doctor or nurses may have already asked you this question: How distressed have you felt over the past week on a scale of 0 – no distress, to 10 – extreme distress? If you are 4 or over on this scale, then your doctor or nurse needs to know so they can work with you on what support you might need. Check the items on the checklist to get a sense of what might be most strongly influencing how you are feeling.
Ask your doctor for a survivorship care plan that details your treatments and follow up checks. Survivorship care plans typically include a treatment summary, a plan about surveillance and follow up tests, and possible treatment side effects that might occur. Lifestyle tips and wellbeing pointers are also often included. Your doctor may have already provided you with a plan, and if not look at the links in the Appendix about Survivorship for examples you can download. Ask your doctor or nurse to complete this with you at your next visit. Involve your partner or family, so you are all across the plan.
Personal Agency
Personal agency belongs to you. This is your ability to be self-aware in how you are going and what you need, to seek assistance when you need it, and to manage your own health where you can. This does not mean going it alone. It means finding out who is there to help, what you can do yourself and what others can offer, and being an active part of the team.
What can I do? A good first step is to set
survivorship goals that most matter to you. In thinking of the months and years
ahead, what are the health and wellbeing or survivorship goals that you would
like to work towards? These might be goals around physical activity or mental
wellbeing; you may also have goals around urinary control or other physical
symptoms. Strengthening your intimate relationship or perhaps looking to
develop one might be on your list. Once you have your goals clear, then
identify the information and other support you might need to achieve these
goals. Set targets that are achievable and put an action plan in place with a
timeline. Be prepared to be flexible and problem solve as you go along. This
approach will help you to feel more in control of your care and the plan going
forward.
Care Coordination
Care Coordination is about your health care team working together to get you the best care possible in a ‘right place at the right time’ approach. It means the team of different types of doctors, nurses and allied health who are looking after you are working together and communicating effectively.
What can I do? Ask your doctor or prostate cancer specialist nurse who is the lead person coordinating your care and to give you a list of all the people who are in your health care team, what their job is, and how you can contact them if you need to. Also, ask who is keeping your family doctor in the loop. If you move to a different treatment approach you might need to ask these questions again.
Evidence-based Survivorship Interventions
Your time and energy are valuable. Being evidence-based is about directing your time, energy and resources to strategies that have strong evidence to support their effectiveness. Good evidence is available for the effectiveness of a range of emotional and mental wellbeing approaches, and this book includes many of these evidence-based strategies. As discussed earlier, there is excellent evidence for the benefits of exercise medicine. And for overall wellness, good nutritional habits are important. Sexual health support tailored to individual men in different age groups and with different sexual orientations and partner relationships is also an area where good evidence exists about what works, and the evidence here continues to grow.
What can I do? The tip here is to be
discerning about the strategies you use to achieve your survivorship goals.
When you consult practitioners, either personally or by sourcing self-help
programs, check the evidence they have to back up their claims of how this
might help you. If you are unsure about this contact a reputable cancer
organisation such as those listed in the Appendix of this book and ask for
advice. There will be different ways to get this type of support, and this
could include face-to-face services, telehealth, web-based programs or
self-help guides. Talk to other men who have had prostate cancer to see what
they have found helpful and accessible. Tap into this valuable resource of
personal experience.
Conclusion
Facing the Tiger: A Survivorship Guide for Men
with Prostate Cancer and their Partners
Professor Suzanne Chambers AO
Reproduction of this article in print or digital form is permitted with the following credit:
'Extract from Facing the Tiger: A Survivorship Guide for Men with Prostate Cancer, ISBN 9781925644425. Copyright Professor Suzanne Chambers AO. Reproduced with permission.'
